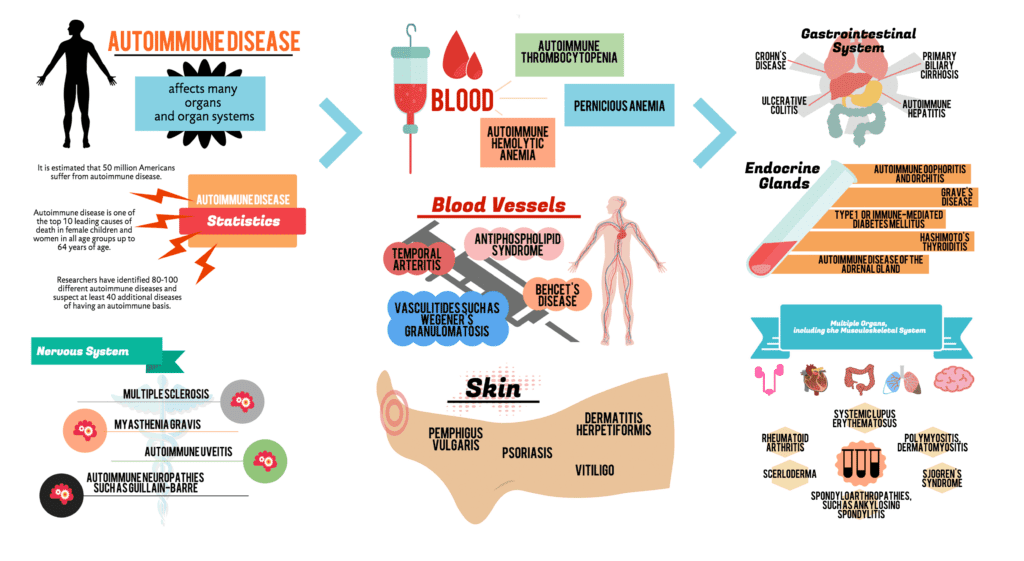
When we look at a person that is not well, one of the first questions needs to be, “what’s the mechanism”. One of the main mechanisms is an autoimmune mechanism, and we’ll talk about how to test for antibodies, and to follow these up with immune panels and specific antigen testing to discover the cause.
Both approaches are like throwing a sandwich to a man being attacked by a pack of wolves; even if your intent was to help him, he has bigger problems than hunger.
Let’s face it, if either traditional medical or the alternative models had any great percentage of success treating autoimmune disease, you wouldn’t be on my web site looking for answers.
It is important to remember that an autoimmune disease is a'state'that the immune system is in. It is not a disease of an organ; and even though it is given a multitude of names depending on the tissue currently affected, it is a state of the immune system attacking the tissue it was meant to protect.
When we look at any thyroid loss of function, we know that the metabolic rate of the person will decrease over time. We know that thyroid hormones have very powerful effects on controlling the metabolism which enables the body to attain homeostasis – a balance of health.* This is why when people are truly hypothyroid, their cellular metabolic rate decreases, they cannot produce the energy in the mitochondria and they have a very hard time attaining a balance in their well-being; their response to viruses and bacteria may diminish, they struggle recovering after stress, just don’t feel as well as they used to and have very low energy. Many of these symptoms come on gradually and if the person is in their thirties or older when the attack takes its hold, they often chock it up to symptoms of aging.
We also know that when a person has thyroid problems they have a diminished gastrointestinal motility, with sluggish gastrointestinal tracts, and they’re often diagnosed with deficiencies in digestive enzymes when the reality is that the body doesn’t have enough metabolic capacity to move food along so there’s fermentation, bloating, gas and constipation. This leads to re-absorption of intestinal toxins and intestinal permeability. This problem is true for many other autoimmune conditions, since many end up attacking parasympathetic nervous centers in the brain that control peristaltic motion.
Another common lab finding with all autoimmune conditions and most certainly in Hashimoto’s patients is that their serum gastrin levels are low. This is an obvious sign of hypochlorhydria or a deceased production of hydrochloric acid in the stomach. There exist strict influences between loss of thyroid activity and gut function.
We also know that when people are autoimmune, several anemias become more probable for developing. One of them is the microcytic hypochromic anemia associated with iron deficiency. Many times when people have low thyroid function, they become iron anemic because they lose ability to absorb iron (and a variety of other nutrients) due to the gut connection listed above. Their slowed intestinal motility has irritated the absorption sites in the small intestines and decreased the ability of enzyme reactions necessary in bringing these nutrients across the gut wall. The decreased intestinal motility also breeds biological attacks in the gut where opportunistic organisms take advantage of static food sources and wreak havoc.* The decreased movement of fecal matter also leads to leaks in the gut membranes and systemic infections that remain ‘low-grade’ and sub-clinical. Then, to make matters worse, because their metabolic rates are down, these people don’t respond well to iron supplements and they often bring about further constipation and misery. What a mess!
Another type of anemia that is common with autoimmune patients are the normocytic-normochromic anemias. This is when the hemoglobin, hematocrit, and RBC levels are depressed but the MCV, MCH and MCHC are normal. Many things can cause normocytic-normochromic anemia, but one of the possibilities is always autoimmune disorder.
Pernicious anemia is an autoimmune attack against a chemical called Intrinsic Factor which is the agent personally responsible for the absorption of vitamin B12. It is not uncommon to see someone that has one autoimmune condition and pernicious anemia, another named autoimmune disease at the same time since the diagnosis of autoimmune disease is named after the organ it is attacking, and the attack has no end if the treatment is centered on suppressing symptoms.

